Get the free soap notes pdf form
Show details
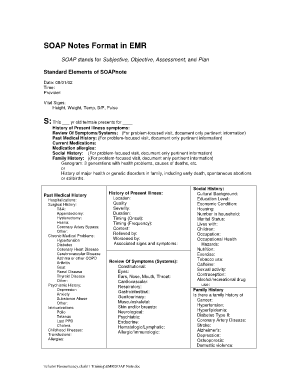
2. Be aware that the following information that should be recorded in your SOAP/CHEAP notes Note any change or lack of change in mental status. Please check with your attending/resident regarding the preferred progress note format either SOAP or CHEAP Chief complaint History Exam Assessment and Plan. Note patient s behavior. Note positive diagnostic studies. Summarize consultations. Note treatment plan with some justification of the treatment described. Note medications dosages and the effect...
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign
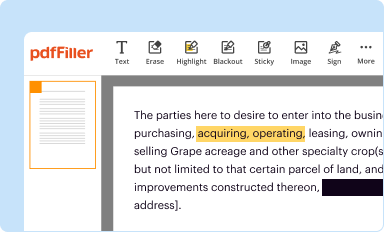
Edit your soap notes pdf form form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
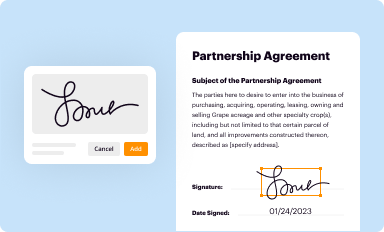
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
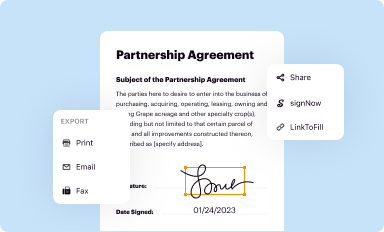
Share your form instantly
Email, fax, or share your soap notes pdf form form via URL. You can also download, print, or export forms to your preferred cloud storage service.
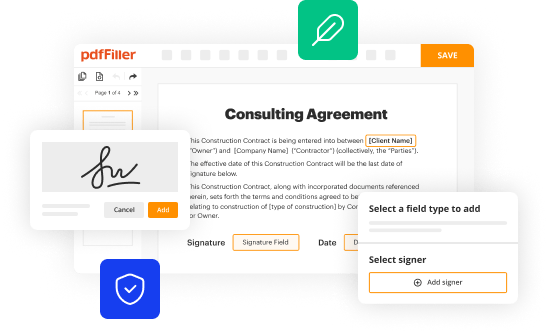
How to edit soap notes pdf online
To use our professional PDF editor, follow these steps:
1
Log in to account. Start Free Trial and sign up a profile if you don't have one yet.
2
Upload a file. Select Add New on your Dashboard and upload a file from your device or import it from the cloud, online, or internal mail. Then click Edit.
3
Edit soap format for progress notes. Text may be added and replaced, new objects can be included, pages can be rearranged, watermarks and page numbers can be added, and so on. When you're done editing, click Done and then go to the Documents tab to combine, divide, lock, or unlock the file.
4
Save your file. Select it in the list of your records. Then, move the cursor to the right toolbar and choose one of the available exporting methods: save it in multiple formats, download it as a PDF, send it by email, or store it in the cloud.
With pdfFiller, it's always easy to deal with documents.
How to fill out soap notes pdf form
How to fill out soap notes pdf?
01
Start by opening the soap notes pdf on your computer or mobile device.
02
Begin by entering the patient's demographic information, including their name, date of birth, and contact details.
03
Move on to the subjective section, where you document the patient's complaints, symptoms, and medical history.
04
Next, describe the objective findings, such as vital signs, physical examination results, and any laboratory or imaging test results.
05
Proceed to the assessment section, where you analyze the patient's condition and make a diagnosis.
06
Finally, outline the plan, which includes the recommended course of treatment, medications prescribed, and any follow-up appointments or referrals.
Who needs soap notes pdf?
01
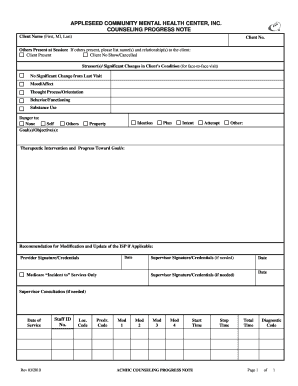
Healthcare professionals, including doctors, nurses, and therapists, use soap notes pdf to document patient encounters and ensure comprehensive and accurate medical records.
02
Medical students and trainees may also use soap notes pdf to practice their documentation skills and learn how to structure clinical notes effectively.
03
Insurance companies and other third-party payers often require soap notes pdf as part of the billing and reimbursement process, to verify the medical necessity of services provided.
Fill form : Try Risk Free
People Also Ask about soap notes pdf
What is the format for SOAP patient notes?
How do you make easy SOAP notes?
How do I create a SOAP note template?
What is the format of a SOAP note?
How do I create a SOAP note?
What is SOAP format template?
Our user reviews speak for themselves
Read more or give pdfFiller a try to experience the benefits for yourself
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
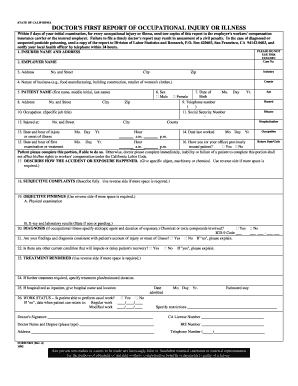
Who is required to file soap notes pdf?
Soap notes are typically filed by healthcare providers such as doctors, nurses, physical therapists, or other medical professionals who are providing patient care.
How to fill out soap notes pdf?
1. Start by writing the patient’s name and some basic information such as date, age, gender, etc.
2. Next, list the chief complaint. This should be the patient’s reason for visiting.
3. After the chief complaint, list the subjective information. This should include the patient’s description of their symptoms, thoughts, feelings, etc.
4. Next, list the objective information. This should include any physical findings that the healthcare provider observed during the visit.
5. After the objective information, list the assessment. This should include any diagnosis made and any other relevant medical information.
6. Finally, list the plan. This should include any treatments, medications, referrals, follow-up visits, etc.
7. When finished, review the notes to ensure accuracy and completeness.
What is the purpose of soap notes pdf?
The purpose of soap notes pdf is to provide a written record of patient visits that includes a summary of the presenting problem, the assessment of the problem, the plan for treatment, and any follow-up notes. This format is used by healthcare providers to document and track patient progress, as well as to provide a comprehensive overview of the patient's medical history and condition for other healthcare providers.
What is the penalty for the late filing of soap notes pdf?
The penalty for the late filing of soap notes varies depending on the jurisdiction. Generally, penalties could include fines, suspension or revocation of a license, or other disciplinary action. In some cases, not filing soap notes on time could even be considered an act of medical malpractice.
What is soap notes pdf?
SOAP notes is a method of documentation used in healthcare to organize and record patient information. The acronym SOAP stands for Subjective, Objective, Assessment, and Plan, which describes the four main sections of the note.
The subjective section includes information provided by the patient about their symptoms, history, and current condition. The objective section includes measurable data such as vital signs, lab results, and physical examination findings. The assessment section is where the healthcare provider analyzes and interprets the subjective and objective information to form a diagnosis or impression. The plan section outlines the treatment plan, including medications, procedures, and follow-up actions.
A SOAP notes PDF is simply a form or template designed in a Portable Document Format (PDF) that healthcare professionals can use to document patient encounters using the SOAP format. These PDFs can be printed or filled out digitally, making it easier to maintain organized and standardized patient records.
What information must be reported on soap notes pdf?
SOAP notes should typically include the following information:
1. Subjective: This section includes information provided by the patient about their symptoms, concerns, and any relevant history. It may also include subjective information gathered from the patient's family members or caregivers.
2. Objective: This section includes the healthcare provider's observations and measurements, such as vital signs, physical examination findings, laboratory or diagnostic test results, and the patient's overall appearance. It should be objective rather than subjective.
3. Assessment: In this section, the healthcare provider makes a professional judgment or diagnosis based on the subjective and objective information provided. It may include differential diagnoses or potential causes for the patient's condition.
4. Plan: This section outlines the proposed plan of action for the patient, including any recommended treatments, medications, procedures, or follow-up appointments. It may also include patient education or referrals to other healthcare providers or specialists.
Additional optional sections that may be included in SOAP notes are:
5. Analysis: In this section, the healthcare provider analyzes the assessment data, discusses potential factors contributing to the patient's condition, and develops a strategy for addressing them.
6. Recommendations: This section includes additional suggestions for the patient's care or self-management, such as lifestyle modifications, home exercises, or dietary recommendations.
NOTE: The specific format and content of SOAP notes may vary depending on the healthcare provider's preferences and the requirements of the healthcare setting or electronic medical record system being used.
Can I create an electronic signature for the soap notes pdf in Chrome?
Yes. By adding the solution to your Chrome browser, you may use pdfFiller to eSign documents while also enjoying all of the PDF editor's capabilities in one spot. Create a legally enforceable eSignature by sketching, typing, or uploading a photo of your handwritten signature using the extension. Whatever option you select, you'll be able to eSign your soap format for progress notes in seconds.
Can I create an electronic signature for signing my fillable soap notes in Gmail?
It's easy to make your eSignature with pdfFiller, and then you can sign your soap note fillable form right from your Gmail inbox with the help of pdfFiller's add-on for Gmail. This is a very important point: You must sign up for an account so that you can save your signatures and signed documents.
How do I edit soap notes pdf straight from my smartphone?
Using pdfFiller's mobile-native applications for iOS and Android is the simplest method to edit documents on a mobile device. You may get them from the Apple App Store and Google Play, respectively. More information on the apps may be found here. Install the program and log in to begin editing soap format for progress notes.
Fill out your soap notes pdf form online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Fillable Soap Notes is not the form you're looking for?Search for another form here.
Keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.